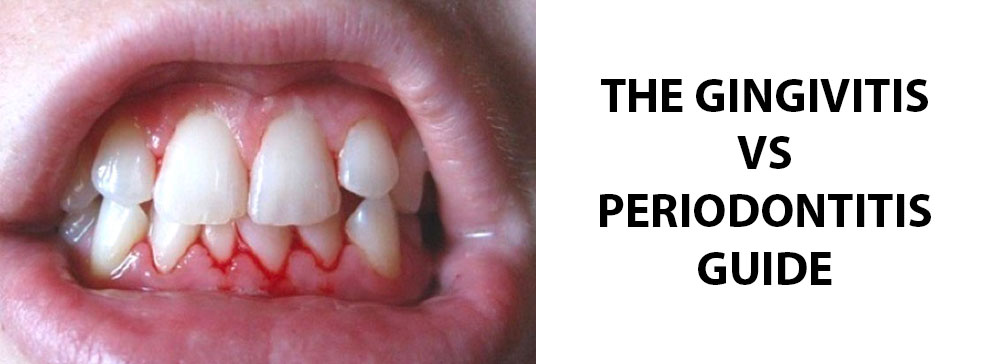
In understanding oral health, recognizing the difference between gingivitis vs. periodontitis is important. While both conditions share common symptoms like swollen, red gums, and bleeding during brushing, gingivitis is generally less severe and often manageable with regular dental care. On the other hand, periodontitis represents a more advanced stage of gum disease, potentially leading to more significant health concerns if left untreated. This basic awareness of their severity can help in maintaining overall oral and general health. If you live in Utah and need help with your periodontitis or gingivitis, we can help. We have multiple offices in the Salt Lake area for you to visit. Click the button below to request an appointment.
What is Gingivitis?
Gingivitis is a common and mild form of gum disease (periodontal disease) that causes irritation, redness, and swelling of your gingiva, the part of your gum around the base of your teeth. It’s important to take gingivitis seriously and treat it promptly.
What Causes Gingivitis?
Gingivitis is primarily caused by poor oral hygiene, which allows plaque—a soft, sticky film of bacteria—to accumulate on the teeth and harden into tartar. This buildup can lead to inflammation of the surrounding gum tissues. Here are the key factors that contribute to the development of gingivitis:
- Plaque Formation: Plaque is constantly forming on your teeth. It’s a mix of bacteria, food particles, and saliva. If plaque is not removed by daily brushing and flossing, it can harden into tartar, a calcified material that plaque adheres to and continues to irritate the gums.
- Tartar Buildup: Tartar (calculus) makes plaque more difficult to remove, creates a protective shield for bacteria, and causes irritation along the gum line. You need professional dental cleaning to remove tartar.
- Gum Inflammation: The longer plaque and tartar remain on the teeth, the more they irritate the gingiva, leading to inflammation.
Signs and Symptoms of Gingivitis
Gingivitis is often characterized by signs and symptoms that are noticeable in the gums. Common signs and symptoms of gingivitis include:
- Swollen or Puffy Gums: One of the most common signs of gingivitis is gums that are swollen and appear more prominent than usual.
- Soft, Receding Gums: The gums might pull away from the teeth, making the teeth look longer than normal.
- Tender Gums: Gums may feel tender when touched or while brushing and flossing.
- Bleeding Gums: Another hallmark of gingivitis is bleeding gums, especially after brushing or flossing your teeth.
- Redness of Gums: Healthy gums are typically a pale pink color, but with gingivitis, they may appear bright red or purple.
- Bad Breath: Persistent bad breath (halitosis) or a bad taste in the mouth can also be indicators of gingivitis.
- Pain When Chewing: In some cases, gingivitis can cause discomfort or pain during chewing.
- Sensitive Teeth: As gums recede due to inflammation, teeth may become more sensitive, particularly to hot or cold temperatures. It’s important to note that in its early stages, gingivitis can be painless and therefore easy to overlook.
What is Periodontitis?
Periodontitis is a serious gum infection that damages the soft tissue and, without treatment, can destroy the bone that supports your teeth. It’s often a progression from gingivitis. Periodontitis leads to teeth loosening or loss, and it’s a common but preventable cause of tooth loss in adults.
What Causes Periodontitis?
Periodontitis is a complex oral health condition with various contributing factors. Here is a list of common causes:
- Plaque Accumulation: The primary cause of periodontitis is the buildup of plaque.
- Tartar (Calculus) Formation: If plaque is not removed, it can harden into tartar, which further irritates the gum tissues.
- Gum Inflammation and Infection: Chronic inflammation caused by plaque and tartar can lead to the infection of the gums and the structures supporting the teeth.
- Body’s Immune Response: The body’s attempt to remove the infection can actually break down the supporting structures of the teeth, including bone and connective tissue.
- Poor Oral Hygiene: Inadequate brushing and flossing make it easier for plaque to accumulate and cause periodontitis.
- Smoking and Tobacco Use: These habits are known to contribute to the development and progression of periodontitis.
- Genetic Factors: Some individuals are genetically predisposed to periodontitis, regardless of their oral hygiene practices.
- Hormonal Changes: Hormonal fluctuations, such as those during pregnancy, puberty, and menopause, can make gums more sensitive to periodontitis.
- Medical Conditions: Conditions like diabetes, which affect the body’s ability to use sugar, can also increase the risk of periodontitis.
- Certain Medications: Some drugs, especially those that reduce saliva flow or cause abnormal growth of gum tissue, can contribute to the development of periodontitis.
- Nutritional Deficiencies: Poor nutrition, especially a lack of essential vitamins and minerals, can weaken the gums and other oral tissues, making them more susceptible to periodontitis.
Signs and Symptoms of Periodontitis
Periodontitis presents with more severe signs and symptoms than its precursor, gingivitis. These symptoms are important indicators of the condition and can include:
- Gum Recession: One of the most noticeable signs of periodontitis is gum recession. This is where the gums pull away from the teeth, making them appear longer. This recession can create pockets between the teeth and gums, where food particles and bacteria can accumulate.
- New Spaces Developing Between Your Teeth: As periodontitis progresses, it can lead to the destruction of the supporting bone structure, resulting in the formation of new spaces or gaps between your teeth.
- Pus Between Your Teeth and Gums: The presence of pus is a clear sign of infection and a classic symptom of advanced periodontitis.
- Persistent Bad Breath: Due to the accumulation of bacteria in the mouth, individuals with periodontitis often experience persistent bad breath, which can be difficult to control even with regular brushing and mouthwash use.
- Bleeding Gums: Similar to gingivitis, bleeding gums during brushing, flossing, or biting into hard food is a common symptom of periodontitis.
- Loose or Shifting Teeth: As the disease progresses, the fibers and bone supporting your teeth are destroyed, which can cause teeth to become loose or shift in your mouth. This can affect how your teeth fit together when you bite and may change the fit of partial dentures.
- Painful Chewing: The weakening of tooth support and inflammation of the gums can make chewing painful.
- Swollen, Red, or Tender Gums: The gums may be swollen, bright red or purplish, and tender, although pain might not always be present.
Treatment for Gingivitis:
- Professional Dental Cleaning: The first step in treating gingivitis is to have a professional cleaning at a dental office. A dentist or dental hygienist will remove plaque and tartar from above and below the gum line. This cleaning is crucial because tartar can only be removed with professional dental instruments.
- Improved Oral Hygiene: Patients are advised to brush their teeth at least twice a day with fluoride toothpaste and floss daily. This helps remove plaque, the primary cause of gingivitis.
- Antibacterial Mouthwashes: Dentists may recommend therapeutic mouthwashes that contain antibacterial properties to reduce plaque and gingivitis.
- Routine Dental Check-ups: Regular dental visits for cleaning and monitoring help keep gingivitis at bay and prevent its progression to periodontitis.
Treatment for Periodontitis:
- Scaling and Root Planing (Deep Cleaning): This non-surgical procedure involves a thorough cleaning of the root surfaces to remove plaque and tartar from deep periodontal pockets and to smooth the tooth root to remove bacterial toxins.
- Medications: Depending on the severity, antibiotics or antimicrobial mouthwashes may be prescribed to manage infection and inflammation.
- Surgical Treatments: In advanced cases, periodontal surgery might be necessary. Options include:
- Flap Surgery/Pocket Reduction Surgery: To reduce the periodontal pocket depth, the gums are lifted back, and tartar is removed. The gums are then sutured back in place to fit snugly around the tooth.
- Bone and Tissue Grafts: Grafting is used to regenerate any bone or gum tissue lost to periodontitis. Bone grafting, for instance, involves using fragments of your own bone, synthetic bone, or donated bone to replace bone destroyed by periodontitis.
- Laser Treatment: Some dentists use laser therapy to remove inflamed gum tissue and reduce the size of periodontal pockets.
- Maintenance Therapy: Following treatment, maintenance therapy is critical. This includes more frequent cleanings (usually every 3-4 months) and careful home care.
Risk Factors of Periodontitis and Gingivitis
- Poor oral hygiene
- Cavities or tooth decay
- Tooth extractions
- Stress
- Nicotine and tobacco
- Vaping
- Certain medications that affect saliva production
- Mouth breathing
- Heart disease
- Type 2 diabetes
- HIV/Aids
- Hormonal changes
- Obesity
- Genetic disorders
- Getting older in age
- Poor nutrition
How to Prevent Gum Disease
- Maintain Good Oral Hygiene: Brush your teeth at least twice a day with fluoride toothpaste. This helps remove the plaque that can lead to gum disease. Make sure to brush along the gum line as well as the teeth.
- Floss Daily: Flossing removes plaque and food particles from between the teeth and under the gum line, where a toothbrush can’t reach.
- Regular Dental Check-ups and Cleanings: Visit your dentist regularly for professional cleanings and oral exams. Dentists can detect early gum disease symptoms and can provide treatment to prevent further progression.
- Quit Smoking and Tobacco Use: Smoking is strongly associated with the onset of gum disease. Quitting smoking can help prevent gum disease or improve the outcome of treatment if you already have it.
- Eat a Balanced Diet: A well-balanced diet, rich in essential nutrients, can boost your immune system and help your body fight off infections, including gum disease.
- Use Therapeutic Mouthwash: Over-the-counter mouthwashes that carry the ADA (American Dental Association) seal can help reduce plaque and prevent or reduce gingivitis.
- Manage Related Health Conditions: Conditions like diabetes can increase the risk of gum disease. Managing these conditions can help prevent the development of gum problems.
- Reduce Stress: Stress can make it harder for your body to fight off infections, including periodontal diseases.
- Avoid Grinding or Clenching Teeth: These habits can put excessive force on the supporting tissues of the teeth and could increase the rate at which these tissues are destroyed.
- Stay Hydrated: Drinking plenty of water helps keep your mouth clean and reduces plaque by washing away food particles and bacteria.
How a Periodontist Can Help
A periodontist specializes in the prevention, diagnosis, and treatment of periodontal disease, and in the placement of dental implants. They are experts in the treatment of oral inflammation and receive extensive training in these areas, including three additional years of education beyond dental school. Periodontists are well-equipped to handle complex periodontal cases, particularly those involving severe gum disease or complex medical histories.
The Gingivitis vs. Periodontitis Guide Conclusion
Understanding the differences between gum diseases like gingivitis and periodontitis is a good idea for maintaining oral health. From recognizing the signs and symptoms to knowing the risk factors and best treatment options, this knowledge plays an important role in preventing and managing these conditions. Good oral hygiene, regular dental visits, and lifestyle choices are key to preventing gum diseases. However, in cases where specialized care is required, the experience of a periodontist becomes necessary.
At Utah Periodontal Specialists, we are dedicated to providing exceptional periodontal care to those in Northern Utah. With our offices located in South Jordan and Salt Lake City, we offer a comprehensive range of periodontal treatments. From non-surgical approaches to advanced surgical procedures, our treatments are customized to meet the unique needs of each patient. Our team of skilled periodontists is committed to ensuring that you receive the highest quality care, incorporating the latest advancements in periodontal treatment.
Recent Comments