Gum disease affects between 20 to 50% of adults worldwide. But what is periodontitis? This serious gum infection can quietly damage your oral health if left untreated. Often beginning as a mild gum inflammation (gingivitis), periodontitis progresses to affect the deeper structures that support your teeth, including the bone.
In this guide, we’ll explain what periodontitis is, what causes it, and how to treat and prevent it. If you’re in need of periodontal treatment, you can count on Utah Periodontal Specialists to take care of your oral health. If you need a periodontist in Utah, we have offices in Salt Lake City and South Jordan and offer competitive prices! Our offices are conveniently located near Bountiful, West Valley, West Jordan, Sandy, Draper, and Murray.
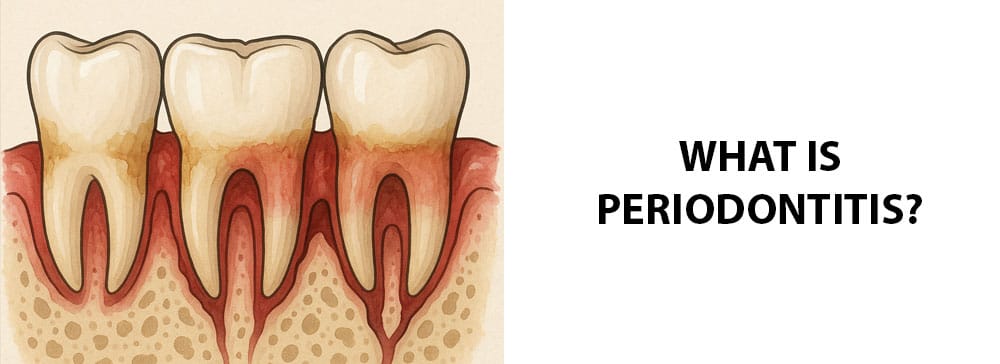
What Is Periodontitis?
What is periodontitis? It’s a serious gum infection that damages the soft tissues and destroys the bone that supports your teeth. Periodontitis is the advanced stage of gum disease that follows gingivitis. It can lead to tooth loss if left untreated. While periodontitis is common in adults, it can be prevented with good oral hygiene.
Periodontitis Symptoms
Periodontitis can develop gradually and usually starts with mild symptoms that worsen over time. Gums that are healthy are firm and range in color from light pink to dark pink or brown. Symptoms of periodontitis often start with changes in the gums. Here are the key signs to watch for:
- Red, swollen, or tender gums
- Bleeding gums, especially when brushing or flossing
- Bad breath that doesn’t go away (halitosis)
- Bad taste in the mouth
- Receding gums, which make your teeth appear longer
- Formation of deep pockets between teeth and gums
- Pus in the gums
- Pain when chewing
- Loose or shifting teeth
- Tooth sensitivity
- Changes in how your teeth fit together
- Spaces developing between teeth
If you notice any of these symptoms, especially bleeding gums or gum recession, it’s important to see a dentist or periodontist as soon as possible. Early treatment can prevent permanent damage.
Diagnosing Periodontitis
A dentist or periodontist will typically diagnose periodontitis by:
- Reviewing medical and dental history: They’ll ask about symptoms like bleeding gums, bad breath, or loose teeth. They will also review risk factors like smoking, diabetes, or a family history of gum disease.
- Visual exam: The dentist will then check for signs of gum inflammation, recession, plaque, and tartar buildup. They’ll look for visible pockets between the teeth and gums.
- Periodontal probing: Using a special instrument called a periodontal probe, the dentist will measure the depth of the gum pockets. Healthy pockets are usually 1 to 3 mm deep. Pockets deeper than 4 mm may indicate periodontitis.
- Dental X-rays: X-rays help detect bone loss around the teeth, which is a key sign of advanced periodontitis. Comparing current and past X-rays can show the progression of the disease.
When to See a Periodontist
A periodontist is a dental specialist who focuses on the prevention, diagnosis, and treatment of gum disease. You should consider seeing a periodontist if:
- You have persistent gum symptoms.
- Your dentist diagnosed or suspects periodontitis.
- You have loose or shifting teeth.
Seeing a periodontist early can help prevent tooth loss and manage your gum health effectively. If you’re experiencing any ongoing gum issues, it’s worth getting a specialist’s opinion.
What Causes It?
Periodontitis is primarily caused by bacterial plaque, a sticky, colorless film that forms on teeth. If not removed by brushing a flossing, plaque hardens into tartar and can lead to infection beneath the gumline. This infection triggers your body’s immune response, which can destroy gum tissue and bone.
How Serious Is It?
Periodontitis is a serious and progressive dental condition that can lead to long-term damage if left untreated. While it usually starts with mild symptoms like bleeding gums, it can quickly escalate into a major oral health problem.
Things You Can Do to Prevent It
Although periodontitis is serious, preventing it is possible with good oral hygiene and regular dental visits. The earlier you take action, the better your chances of avoiding gum disease altogether. To prevent periodontitis, you should:
- Brush your teeth twice a day, using a soft-bristled toothbrush and fluoride toothpaste. Brush for at least 2 minutes, reaching along the gumline where plaque builds up.
- Floss daily to remove plaque and food particles between teeth and under the gums, where your toothbrush can’t reach.
- Get regular dental checkups and cleanings, at least every 6 months. If you’re at high risk, you may need to go in more regularly. Professional cleanings remove tartar, which cannot be brushed away.
- Quit smoking or using tobacco. Tobacco use greatly increases your risk of gum disease and interferes with healing.
- Manage chronic conditions like diabetes, which can make you more vulnerable to infections, including gum disease.
Potential Problems
If left untreated, periodontitis can lead to a range of serious health problems, including:
- Tooth loss: As the gums, bone, and ligaments supporting your teeth break down, teeth can loosen and fall out or need to be extracted.
- Bone loss in the jaw: Periodontitis destroys the alveolar bone around the teeth, weakening the jaw structure, and making it harder to place implants later.
- Gum recession: Gums pull away from teeth, making teeth look longer and exposing sensitive tooth roots.
- Chronic bad breath and taste: Persistent infection in the gums produces foul odors and an unpleasant taste that doesn’t go away with brushing.
- Health problems in other parts of the body: Ongoing inflammation in the gums puts you at higher risk for heart disease, stroke, respiratory infections, and pregnancy complications.
Surgical and Non-Surgical Treatments
Now that we’ve answered the question “What is periodontitis?,” let’s talk about how to treat it. Most treatment plans begin with non-surgical methods. If the disease progresses or does not respond, surgical options may be necessary.
Non-surgical treatments include:
- Scaling and root planing (deep cleaning): Scaling removes plaque and tartar from below the gumline, while root planing smooths the root surfaces so that gums can reattach to the teeth. This is often done under local anesthesia.
- Antibiotic therapy: Topical or oral antibiotics are used to kill bacteria and reduce inflammation. Options include antimicrobial mouth rinses, gels, or pills.
- Good oral hygiene: Patients can prevent recurrence by brushing their teeth twice a day and flossing once a day.
- Maintenance: More frequent dental cleanings (every 3 to 4 months) and regular monitoring of gum health can prevent recurrence or catch issues earlier.
When periodontitis progresses, surgical treatments can include:
- Flap surgery (pocket reduction surgery): The gums are lifted back to remove tartar and reduce pocket depth. Gums are then stitched tightly around the tooth for easier cleaning.
- Bone grafts: Natural or synthetic material is grafted to existing bone structures to replace bone that was destroyed by the disease. This encourages new bone growth and helps stabilize teeth.
- Soft tissue grafts: Tissue from the roof of the mouth or a donor source is used to cover exposed roots. This helps reduce gum recession and protects against further damage.
Conclusion
What is periodontitis? Periodontitis is more than just red and bleeding gums. It’s a serious, progressive infection that, if left untreated, can lead to tooth and bone loss and systemic issues.
If you’re experiencing symptoms like tender gums, loose teeth, or persistent bad breath, it’s a good idea to make an appointment with a periodontist. At Utah Periodontal Specialists, we have a team of experienced specialists who can help you treat your gum disease. Whether you need scaling and root planing or surgical treatment, we offer personalized treatment plans to help you improve your oral health.
Recent Comments